The Economics of Cardiac Device Remote Patient Monitoring
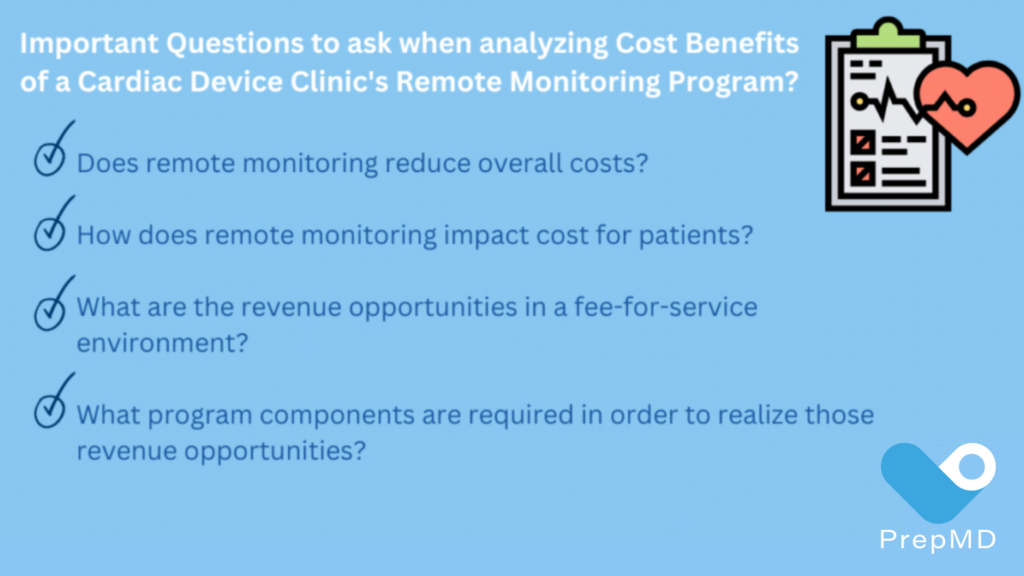
Almost universally, Cardiac Device Clinic Managers face many common challenges and need to tackle some difficult questions when analyzing a CIED remote monitoring program. Many of these questions relate to financial considerations.
 Dr. Lerman, Senior Cardiologist and Physician Executive with decades of experience in both clinical and business aspects of healthcare, outlined some of the most common questions asked by clinic managers as they consider starting a remote monitoring program, “The discussion should always start with patient care and clinical benefits.
Dr. Lerman, Senior Cardiologist and Physician Executive with decades of experience in both clinical and business aspects of healthcare, outlined some of the most common questions asked by clinic managers as they consider starting a remote monitoring program, “The discussion should always start with patient care and clinical benefits.
Key factors to examine when considering the outcome benefits for cardiac device patient remote monitoring include:
-Reduction in mortality amongst heart failure patients
-Reduction in hospitalizations, emergency department visits and office visits
-Decreased time from clinical event to clinical decision
-Early predictors of heart failure exacerbation
-Early detection and quantification of atrial fibrillation”
In 2015, as a result of the many outcomes-benefits studies done over the years, the Heart Rhythm Society designated remote monitoring and interrogation as a Class IA recommendation, when combined with at least one annual in-person evaluation. Furthermore, all patients should be offered remote monitoring as part of the follow-up management strategy when technically feasible.
So, what are the costs associated with achieving the clinical outcome advantages of a remote monitoring program? Any program that enhances patient outcomes should garner support when the economics are neutral or positive. However, programs that significantly escalate costs may face challenges in gaining traction, even if they offer patient benefits.
While cost is important, the overall economic picture depends largely on whether the clinical program exists in a fee-for-service or so-called “fee-for-value” environment (managed care, accountable care organizations, etc.)
In fee-for-service environments, revenue generation is balanced against cost. In fee-for-value, cost reduction is the primary economic driver, as it can lead to shared savings from payors. Complicating matters is that the long awaited transformation from fee-for-service to fee-for-value is still largely a work in progress, and most organizations are somewhere in the middle with participation in both types of financial arrangements. When addressing remote monitoring, it is important to consider the following questions:
One way to answer the first question is through formal health economics research, but those studies can be very challenging, especially when trying to decide how much to value studies done abroad or in a different reimbursement or healthcare climate. The TARIFF Study1 is one frequently referenced Italian study published in 2017, which showed that remote monitoring resulted in statistically significant reductions in hospitalizations, emergency visits, outpatient diagnostic tests, and clinical evaluations compared with standard care. The overall mean annual cost per patient in the remote monitoring group was 54% lower than standard care, driven primarily by a lower cost of cardiovascular hospitalizations. This cost reduction is consistent with the hypothesis that earlier identification of clinical or device issues will result in earlier intervention and less complicated hospitalizations.
Another relevant study published in 2021 in the Canadian Journal of Cardiology2 followed ICDs and CRT-D patients for an average of 50 months. The data showed that remote monitoring was associated with both a lower risk of death and cardiovascular hospitalizations, with cost savings observed over five years of over $12,000 per patient. In summary, while the evidence that remote monitoring lowers overall costs is not as strong as the clinical outcomes evidence, there is little evidence suggesting that costs will be increased.
“Device Clinic managers can reasonably conclude that implementing a high quality remote monitoring program will result in improved patient care and better clinical outcomes, with a cost-neutral or possible reduction in overall costs to the clinic or hospital,” explained Dr. Lerman
As important as it is to evaluate the economic impact of remote monitoring on the healthcare organization, it is just as critical to consider the impact on individual patients. A 2021 American Journal of Cardiology article3 described how cardiac device patients frequently express concerns over remote monitoring, cost transparency, and billing.
 Kent Seckinger, CCDS, PrepMD Customer Success Director, discussed how to best approach these common patient concerns. “What it really comes down to is patient education and transparency. Educating the device patients is critical to ensuring that they know that there are real benefits for them with remote monitoring. A discussion with each patient should include the specifics of the billing model and relevant regional reimbursement rates, and most importantly, an explanation of the clinical benefits realized with remote monitoring, such as reduction of hospitalizations and ER visits.”
Kent Seckinger, CCDS, PrepMD Customer Success Director, discussed how to best approach these common patient concerns. “What it really comes down to is patient education and transparency. Educating the device patients is critical to ensuring that they know that there are real benefits for them with remote monitoring. A discussion with each patient should include the specifics of the billing model and relevant regional reimbursement rates, and most importantly, an explanation of the clinical benefits realized with remote monitoring, such as reduction of hospitalizations and ER visits.”
Patients better understand remote monitoring costs when they grasp the clinical rationale and benefits. Without this patient education, patients often call the clinic in frustration when they receive bills that they don’t understand, increasing staff burden. Even worse, they may decide to disconnect their monitors. It is crucial to discuss remote monitoring with the patient and their family members no later than the very first visit immediately after implantation. This ensures that they understand its importance and implications from the outset
Seckinger explained that the PrepMD Clinic Solutions Team have found that a little patient education goes a long way. “The patient often feels they’ve taken ownership in the management of their care as well. A critical 30-minute discussion on the benefits of remote monitoring with the patient at their first visit will definitely save time in the long run.”
While the primary motivation to provide remote monitoring services for CIEDs is to provide the highest quality patient care, organizations that participate in fee-for-service environments have an opportunity for increased revenue generation. That is because remote monitoring best practices involve improving patient compliance, which along with a detailed understanding of billing requirements, typically leads to a higher overall volume of billable transmissions. ICD transmissions can typically be billed quarterly, pacemakers every 3-6 months, and ILR and heart failure monitoring can often be billed monthly. This increased transmission volume usually more than compensates for the costs incurred by a third party remote monitoring service if one is utilized. Although there is still a fair amount of regional differences in reimbursement for some remote monitoring services, typically, a well run and legally compliant program is profitable.
It is important however, to be cognizant of the cost burden of remote monitoring on patients, especially for Implantable Loop Recorders (ILRs) and devices where heart failure monitoring can be performed and billed. In both of these circumstances, Medicare allows billing for 30-day monitoring periods, and while such billing meets regulatory requirements when clinically indicated, patient co-payments can add up quickly, especially in regions with high reimbursement.
Greg O’Neal, CCDS, CEPS, PrepMD Director of Technology and Business Development discussed the 2015 HRS Expert Consensus Statement4 of remote interrogation and monitoring for cardiovascular implantable electronic devices. The HRS consensus statement described a cadence of regularly scheduled quarterly remote monitoring transmissions for pacemakers and implantable defibrillators (monthly for ILRs and insertable cardiac monitors) with ad hoc in-person evaluations based on device or patient generated alerts plus a single scheduled annual in-person evaluation, all of which can be potentially reimbursable.
In developing a fee-for-service model, a clinic must be able to optimize the frequency of the remote monitoring transmissions with the appropriate CPT code usage for each device type, including the professional and technical components, while keeping all the patient transmission schedules consistent on each of the vendor websites for all devices.
 Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
Greg O’Neal, PrepMD Director of Product & Business Development explained, “In general, we find that many clinics running remote monitoring programs monitor patients less frequently than optimal. This highlights the discrepancy between the ideal monitoring frequency and the actual practices in clinics. The typical reimbursement is often less than 50% of the optimal.”
Clinics should ensure they use the correct CPT billing codes for monitoring heart failure patients monthly, as this could potentially increase their top-line revenue by 30 to 40%.
In addition to making sure that device transmission schedules are optimized, clinics need to carefully track connectivity and quickly move to restore disconnected monitors and minimize missed transmissions. In-person visits need to be coded properly and remote schedules adjusted if necessary.
Dr. Lerman concluded, “No two clinics are the same and this can make effective clinic remote monitoring management a daunting task. It’s clear that there are opportunities here both on the cost saving side and- if you’re in the appropriate model- on the revenue generation side. However, you can’t just roll out of bed one day and realize both these economic outcome benefits as well as the clinical outcome benefits.”
Clinic managers will find that utilizing these best practice principles will help guide them through the process of implementing and managing an effective remote monitoring program at their clinic:
- Improving Patient Communication and Education
- Monitoring and Ensuring Remote Monitoring Scheduling and Compliance
- Ensuring Appropriate CPT Codes, Billing, and Reimbursement
As far as costs are concerned, device clinics may be able to take advantage of appropriate partnerships to optimize their resources. This may be a combination of training, staffing, remote monitoring software and service in the form of a bundled solution that enables the clinics to manage their costs effectively, enhancing their profitability. By strategically partnering with reliable solution providers such as PrepMD, clinics can ensure they are investing in the most efficient and cost-effective solutions tailored to their specific needs. Such partnerships can help clinics navigate the complexities of budgeting and resource allocation, ultimately leading to greater financial sustainability and success.
Explore companies like PrepMD for comprehensive device clinic solutions and discover how highly experienced and certified professionals can collaborate with your clinic to improve patient care, optimize billing, and manage costs with bundled solutions. Additionally, explore the relevant publications below for further insights.
CITATIONS:
1 Ricci, Renato Pietro, et. al, “Economic analysis of remote monitoring of cardiac implantable electronic devices: results of the health economics evaluation registry for remote follow-up (TARIFF) study,” NIH Comparative Study: Heart Rhythm, 2017 Jan;14(1):50-57. doi: 10.1016/j.hrthm.2016.09.008. Epub 2016 Sep 8, https://pubmed.ncbi.nlm.nih.gov/27614025/.
2Abramson, Beth L., et. al., “Canadian Cardiovascular Society 2022 Guidelines for Peripheral Arterial Disease,” NIH Practice Guideline: Canadian Journal of Cardiology. 2022 Jun;38(6):736-744. doi: 10.1016/j.cjca.2022.01.022. Epub 2022 Jan 29, https://pubmed.ncbi.nlm.nih.gov/35537813/.
3Fraiche, Ariane M., ”Patient and Provider Perspectives on Remote Monitoring of Pacemakers and Implantable Cardioverter-Defibrillators,” Research Article: American Journal of Cardiology Volume 149, P42-46, June 15, 2021, https://www.ajconline.org/article/S0002-9149(21)00266-6/fulltext.
4Slotwiner, David, MD, et. al. 2015 “HRS Expert Consensus Statement of remote interrogation and monitoring for cardiovascular implantable electronic devices.” Heart Rhythm, volume 12, Issue 7, July 2015, Pages e69-e100, https://www.sciencedirect.com/scie